Understanding Disease
Understanding
Cushing's Disease
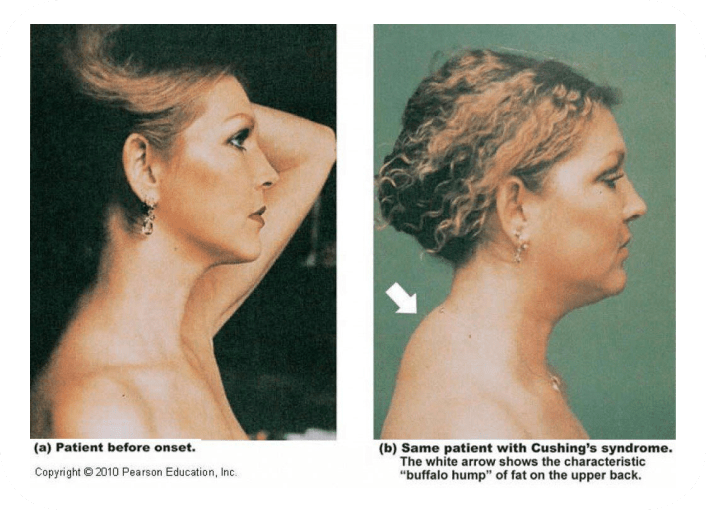
By now you know you have been diagnosed with Cushing’s disease. This rare condition is caused by a noncancerous tumor on the pituitary gland that is located at the base of the brain. The tumor causes the pituitary gland to release too much
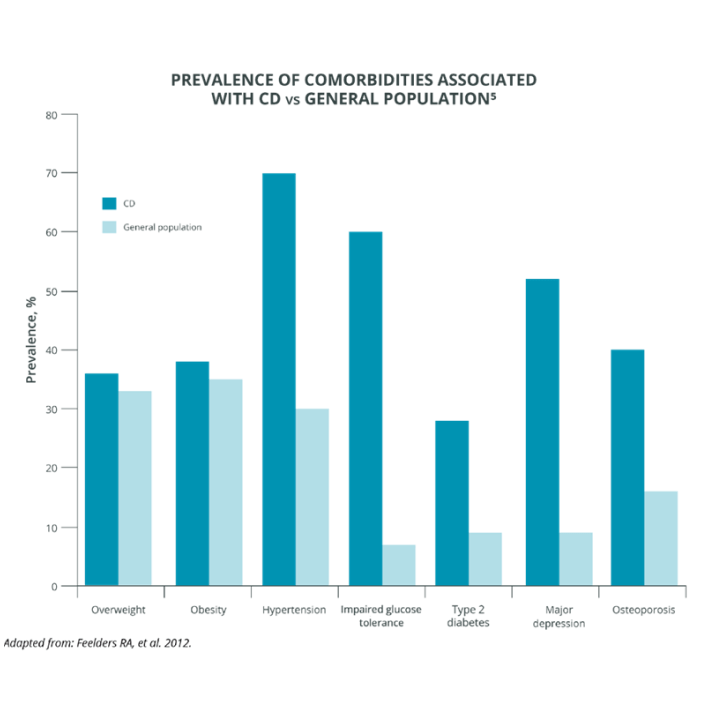
adrenocorticotropic hormone (ACTH). ACTH causes the production and release of cortisol, the stress hormone. Having too much ACTH leads to excess amounts of cortisol in the body, which may lead to a number of health issues.