Symptoms Checker8
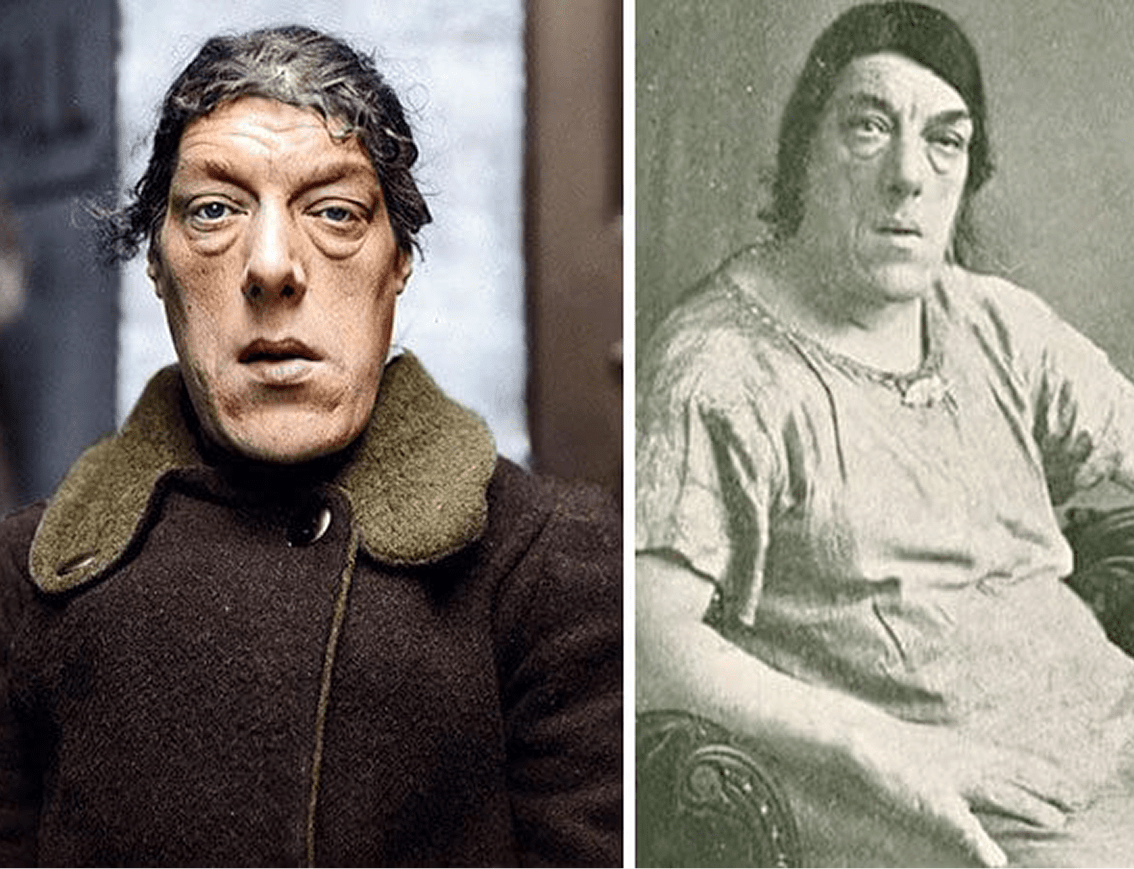
How to Identify the Signs of Acromegaly
Our recorded sessions provide valuable insights from leading healthcare professionals, researchers, and individuals who are living with Acromegaly and Cushing's Disease.
(At least 1 ACRAL & FACIAL FEATURES)
Increase in shoe size
Increase in the size of hands
(Example: patient needed to buy bigger gloves or noticed an increase in ring size and others)
Any abnormal facial features (compared to old photographs)
(Example: swollen lips and tongue, enlarged nose, protruding forehead, protruding lower jaw and others)
(At least 2 or more acromegaly associated comorbidities)
History of or existing Cardiac disease (including biventricular hypertrophy and diastolic or systolic dysfunction)
Carpel tunnel syndrome
Colonic polyps
Diaphoresis (excess perspiration or oily sweating)
Diffuse arthralgia (large joint pains)
Fatigue
Persistent headache
Visual field defects
New-onset or uncontrolled diabetes
New-onset or difficult-to-control hypertension
Amenorrhea
Misalignment of teeth/bite or progressive teeth spacing
Sleep apnoea syndrome (excessive snoring)
Multiple skin tags
You appear to be in good health! Your responses do not currently indicate major symptoms.
Continue to monitor your condition and maintain healthy habits. If new symptoms develop, please reassess or consult a healthcare professional.
Based on your responses, you are showing significant symptoms.
Please visit your nearest Klinik Kesihatan or healthcare provider for further diagnosis and medical advice as soon as possible.
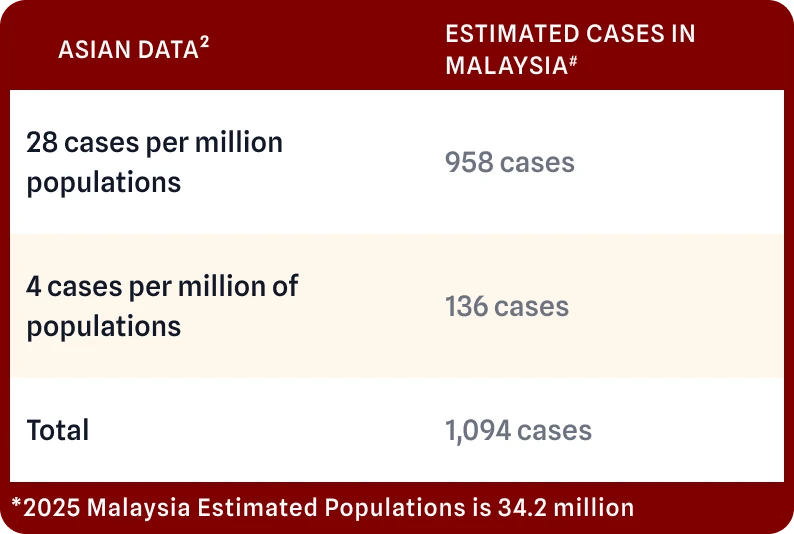
UNDERSTANDING DISEASE
Acromegaly Disease
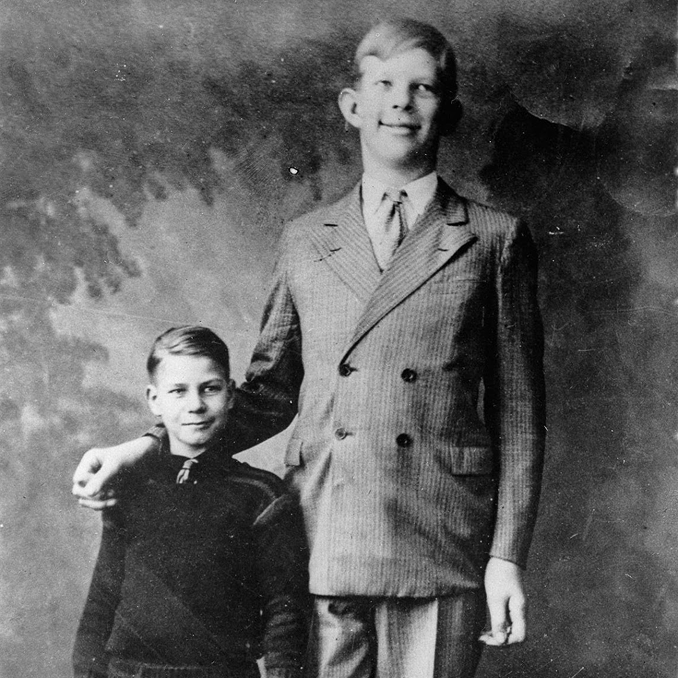
Acromegaly is caused by excess growth hormone - usually from a non-cancerous pea-sized gland called pituitary - and leads to gradual enlargement of the hands, feet, face, and soft tissues, along with serious metabolic and cardiovascular complications that require timely diagnosis and management.
Acromegaly Disease
Disease Development and Impact
Changes are typically slow and progressive over months to years, so symptoms may be subtle early on. Left untreated, acromegaly causes health problems and death through cardiovascular, metabolic, respiratory and vision complications; effective diagnosis and treatment reduce these risks and can halt or partially reverse some features.
Individuals can share their experiences

Prevalence mean age diagnosis 40-50 years old2-4

Affects men and women equally2-3
Causes and Signs & Symptoms
MORE THAN 95% are due to growth hormone secreting pituitary tumours 5
In rare occasion, non-pituitary neuroendocrine tumours that cause ectopic secretion of growth hormone releasing hormone (GHRH) which may be bronchial, pancreatic, gastrointestinal, thymic and tumours associated with Multiple endocrine neoplasia type 1 (MEN1).
Signs & Symptoms
Symptoms often develop slowly and may be missed. Watch for:

Enlarged extremities e.g. hands or feet (Ring no longer fit/changes in shoe sizes)
Facial Changes (Broader nose, protruding lower jaw, broader forehead)

Joint Pain

Headaches or vision

Lower pitch voice

Snoring or fatigue
LEARN MORE
Acromegaly Treatment
Respiratory
You may suffer from sleep apnoea, and snoring. 2,15,16
Skeletal and rheumatological
You may suffer from osteoporosis, vertebral fractures, and painful bone and joint pathologies, which can reduce joint mobility and progress to true osteoarthritis. 2.15
Neurological
Carpal tunnel syndrome, most of-ten nocturnal paraesthesia ("tin-gling") can occur in the hands as a result of damage to the median nerve (in the palm of the hand). 2,16
Why Early Diagnosis Matters
If left untreated, acromegaly can lead to serious complications like:
High Blood Pressure

22.3% – 76.8%9
Type 2 Diabetes

18% –77%9
High Cholesterol

up to 61%9
Overweight

>40%9
